
Osteochondrosis is a degenerative-dystrophic lesion of the spinal column, which leads to the destruction of the intervertebral discs with corresponding consequences. Osteochondrosis "infects" the entire spine, but the symptoms of the disease are most pronounced when the cervical, as the most mobile, and lumbar parts are affected. The chest area suffers the least.
Signs of cervical osteochondrosis are very diverse and often resemble other diseases, which makes differential diagnosis and early recognition of pathology difficult. In this article, we will take a detailed look at how osteochondrosis of the cervical spine manifests itself and what will help you suspect this disease.
Degree of osteochondrosis
Osteochondrosis is a chronic progressive disease that occurs with periods of remissions and exacerbations. Pronounced clinical symptoms do not appear immediately, but after some time, when the degenerative process enters the 2nd or even 3rd stage.
There are only 4 degrees of pathology:
- The initial stage is characterized by pathological changes within the intervertebral disc. It loses moisture, which leads to degenerative changes, reduction in disc height and rupture of the fibrous capsule. There are usually no signs at this stage. Diagnosis is possible only with MRI of the spine. This is the most favorable stage to start treatment, because in this case it is possible to completely restore the damaged discs, which cannot be done in the future.
- Osteochondrosis of the 2nd degree is characterized by worsening of the damage to the intervertebral discs. Their height decreases significantly, which leads to relaxation of the spinal muscles and ligaments. All this causes instability of the damaged segment of the spinal column, increased mobility of the vertebrae, their movement and sliding relative to each other and the axis of the spine. As a rule, in this phase, the first signs of the disease appear in the form of pain and other signs specific to lesions of the cervical spine.
- In the 3rd stage, protrusions and hernias of the intervertebral discs develop. The symptoms of the disease are fully expressed.
- The fourth stage is final. In this case, the formation of osteophytes and deformities of the spine occurs. The body tries to somehow stabilize the damaged segment of the spine, due to which osteophytes develop, ossification of ligaments and other processes that lead to stabilization of the vertebrae, but, unfortunately, this process is accompanied by subluxations of the vertebrae and different types and degrees. spinal deformities.

Nature of symptoms of cervical osteochondrosis
Manifestations of osteochondrosis in the cervical spine are associated with 3 mechanisms of negative impact of this pathology:
- Direct compression of the spinal cord, which flows in the spinal canal. It should be noted that this very rarely happens with an advanced degenerative process and its complications. Compression of the nerve tissue of the spinal cord can be caused by a large intervertebral hernia, which protrudes directly into the lumen of the spinal canal; stenosis (narrowing) of the spinal canal due to degenerative changes; dislocations, subluxations, fractures of damaged vertebrae.
- It has a negative effect on the structures of the peripheral nervous system (spinal cord roots and nerve fibers) that come out of the cervical spine. They can be compressed between adjacent vertebrae or herniated protrusions, and can become inflamed and irritated. All this leads to a series of severe symptoms. This is the most common group of signs of cervical osteochondrosis.
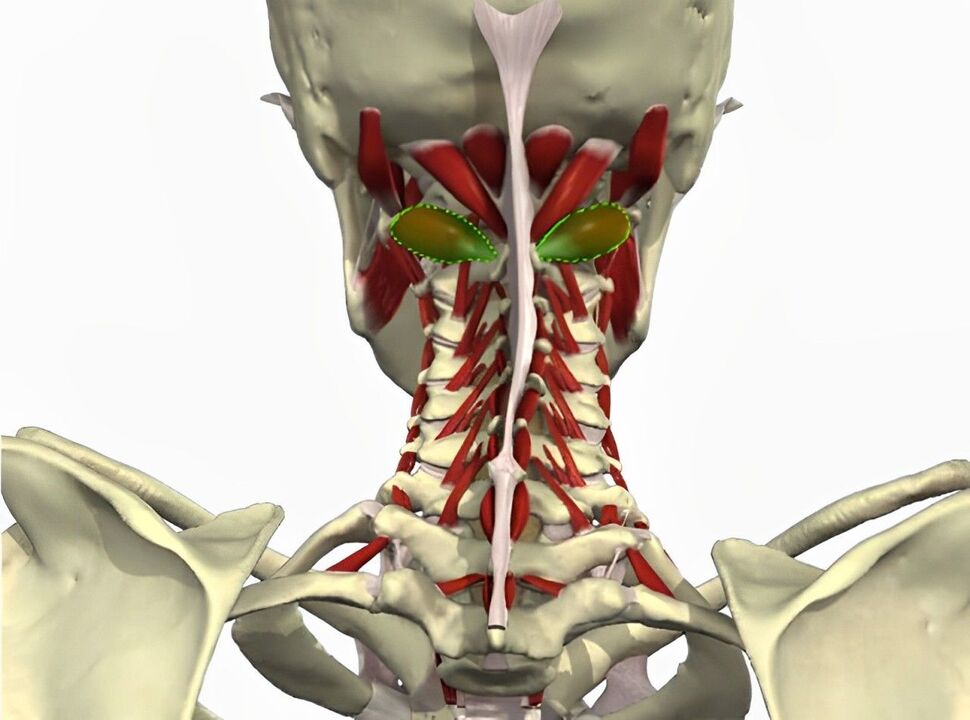
- It has a negative effect on the blood vessels that pass near the damaged area of the spine. Of particular clinical importance is one very important arterial vessel - the vertebral artery, which passes through the openings of the transverse processes of the cervical vertebrae into the skull cavity and supplies blood to the back third of the brain and the cerebellum.
Let's consider in detail each group of mechanisms and which symptoms they cause.
Symptoms associated with spinal cord injury
As already mentioned, compression of the spinal cord in cervical osteochondrosis is very rare. This is a very serious condition that can cost a person not only his health, but also his life.
Damage to the upper part of the cervical spine is life-threatening. The cardiovascular and respiratory centers suffer, which leads to immediate death. With compression at the level of 3-4 segments of the spinal cord, tetraplegia develops (paralysis of all limbs and muscles below the injury). The respiratory muscles and diaphragm also suffer, which can lead to respiratory arrest and death.
If damage occurs at level 4. -5. segment of the spinal cord, tetraplegia develops, but without respiratory impairment. When 5-8 segments of the spinal cord are compressed, different muscle groups of the upper extremities are injured and paraparesis of the legs and disorders of the pelvic organs occur.
Symptoms associated with nerve damage
Pain syndrome
First of all, the pain syndrome should be highlighted, which can be chronic (cervicalgia) and acute in the form of lumbago (cervicalgia). Pain occurs in the neck, occipital part of the head and shoulder girdle. It is usually caused by irritation, compression and inflammation of the nerve roots of the cervical spine, as well as pathological spasm of the muscles in this area that are innervated by these nerves.
The pain associated with cervicalgia is almost constant, painful and varies in intensity. As a rule, the pain syndrome can be tolerated. Appears or increases with sudden movements, turns and tilts of the head. Movements in the neck are accompanied by a characteristic crunching sound.
Pain in the cervix occurs suddenly in the form of a shooting or electric shock. It is very intense, it goes in one hand. It lasts for a few seconds or minutes and then turns into cervicalgia. It is usually caused by sudden movement and compression of the nerve.

Radicular syndromes
All the main nerves of the upper extremity (median, ulnar and brachial) are formed by nerve fibers coming out of the cervical spine. Therefore, in the presence of cervicobrachial osteochondrosis, these nerve structures can suffer. All these nerves are mixed, i. e. they have both sensory and motor function. Depending on which root is affected, symptoms will vary. For example, the sensitivity of the 2nd or 3rd finger may be lost and paralysis of one or more muscles may occur. All these signs of nerve damage are classified into separate syndromes, which can only be determined by a neurologist.
Occipital neuralgia
Occipital neuralgia occurs when the greater and lesser occipital nerves, which are formed by the 2nd, 3rd and 4th pairs of cervical spinal nerves, are damaged. When these structures are compressed, irritated or inflamed due to a degenerative process in the spine, a headache occurs in the back of the head, which women often complain about.
This pain is so typical that only its description allows the correct diagnosis to be made in 90% of cases. It is also called bursting cranialgia. The pain attack occurs suddenly, has a unilateral localization (rarely it hurts on both sides), patients compare the nature of the pain to an electric shock. The attack lasts for a few minutes, but can be repeated several times a day. Pain occurs on the posterolateral surface of the neck and spreads upward to the occipital protuberance (repeats the anatomical course of the occipital nerve). At the same time, a disorder of the sensitivity of the skin of the back of the head (numbness, crawling sensation) may develop.
Cardiac syndrome
This name is due to the fact that this manifestation of osteochondrosis of the cervical spine is very similar to angina pectoris and other heart diseases. The reason for this phenomenon is damage to the nerve fiber that innervates the pectoralis major muscle and the phrenic nerve, whose fibers are woven into the pericardium of the heart.

The cause of the pain is a spasm of the pectoralis major muscle due to pathological impulses along the damaged nerve fiber. At the same time, patients very often confuse such pain with heart pain. In contrast to coronary pain, the pain syndrome in cervical osteochondrosis has a long duration (sometimes several hours or days), which does not happen in angina pectoris, is not related to physical activity, but there is a relationship with body position. The pain increases with sudden movements, turning the head, coughing, sneezing, which does not happen with angina pectoris. Antianginal drugs (nitroglycerin, etc. ) will not be effective.
Important! In any case, such symptoms require a thorough differential diagnosis, because atypical variants of angina and heart attack also occur. In order not to miss a serious illness, you must first do an EKG. In osteochondrosis, no pathological changes will be noted.
Symptoms associated with vertebral artery injury
Compression of the vertebral artery during cervical osteochondrosis can cause a large number of unpleasant manifestations, which are mainly associated with a decrease in blood flow and hypoxia of the part of the brain that is fed by this vessel (back third of the brain and cerebellum).
Signs of vertebral artery syndrome:
- headache of a diffuse or pulsating nature in the back of the head, temples and parietal region;
- dizziness;
- nausea and vomiting;
- visual disturbances;
- ringing in the ears, reduced hearing acuity;
- impaired coordination and balance;
- development of falls (sudden falls without loss of consciousness due to sudden head turns);
- memory impairment, reduced performance, ability to concentrate.
It's important to remember! With pronounced changes in the spine, the artery can be so compressed that it will lead to the development of an ischemic stroke in the vertebrobasilar region of the brain. Therefore, it is important to suspect pathology in time and take all necessary measures to improve the health of the spine and prevent further pathological changes.
FAQ
What symptoms accompany cervical osteochondrosis?
Symptoms of cervical osteochondrosis may include pain and stiffness in the neck, headaches, dizziness, ringing in the ears, and tingling or numbness in the arms and shoulders.
How can you alleviate the symptoms of cervical osteochondrosis?
To alleviate the symptoms of cervical osteochondrosis, it is recommended to engage in physical exercises, maintain proper posture, avoid long-term sitting in one position, use special pillows and mattresses, and use physical therapy methods.
Useful tips
Tip #1
Pay attention to pain in the neck, shoulders and arms, which can be symptoms of cervical osteochondrosis. The pain can be sharp, dull or localized in certain places.
Tip #2
Pay attention to numbness or weakness in the hands, fingers or shoulders, as this may also be due to cervical osteochondrosis.
Tip #3
Pay attention to headaches, dizziness and ringing in the ears, as these symptoms can also be associated with cervical osteochondrosis.












































